Inside Oregon State Hospital
When multiple patients, family members, and staff members raised increasingly urgent concerns about deteriorating conditions at OSH, DRO brought video equipment to gather stories.
Oregon State Hospital (OSH) is an important indicator of how our state is meeting its obligations to provide treatment to patients in its care. OSH is the State of Oregon's public psychiatric hospital.
Since 1986, Disability Rights Oregon (DRO) has been monitoring conditions at OSH. As a watchdog agency, DRO has built relationships with the staff, patients, and their family members. As the federally mandated Protection and Advocacy System for people with disabilities, DRO may monitor any place a person with a disability lives (42 C.F.R. § 51.42).
When multiple patients, family members, and staff members raised increasingly urgent concerns about deteriorating conditions at OSH, DRO brought video equipment to gather stories. The interviews took place between July 15 to September 7, 2022 at both the Salem and Junction City campuses of OSH. DRO would like to thank the patients, clinicians, and family members for sharing their stories with us.
“Please don’t just listen to what you’re hearing from hospital admin. Come talk to us, or give us a way to talk to you that’s safe. Come talk to our patients and their families. They’re human beings. They’re not just numbers.”
— Oregon State Hospital Staff, Anonymous Whistleblower
Stories from the Oregon State Hospital
William & Julie: Family Separated
“Its comical to say that it is a mental health hospital… there is no mental health treatment.”
Mike: a Failed stepdown
“I don’t have any options… just the forced option to go live on the street. I can’t live on the street.”
The Oregon State Hospital
The Erosion of Rights & Quality Treatment
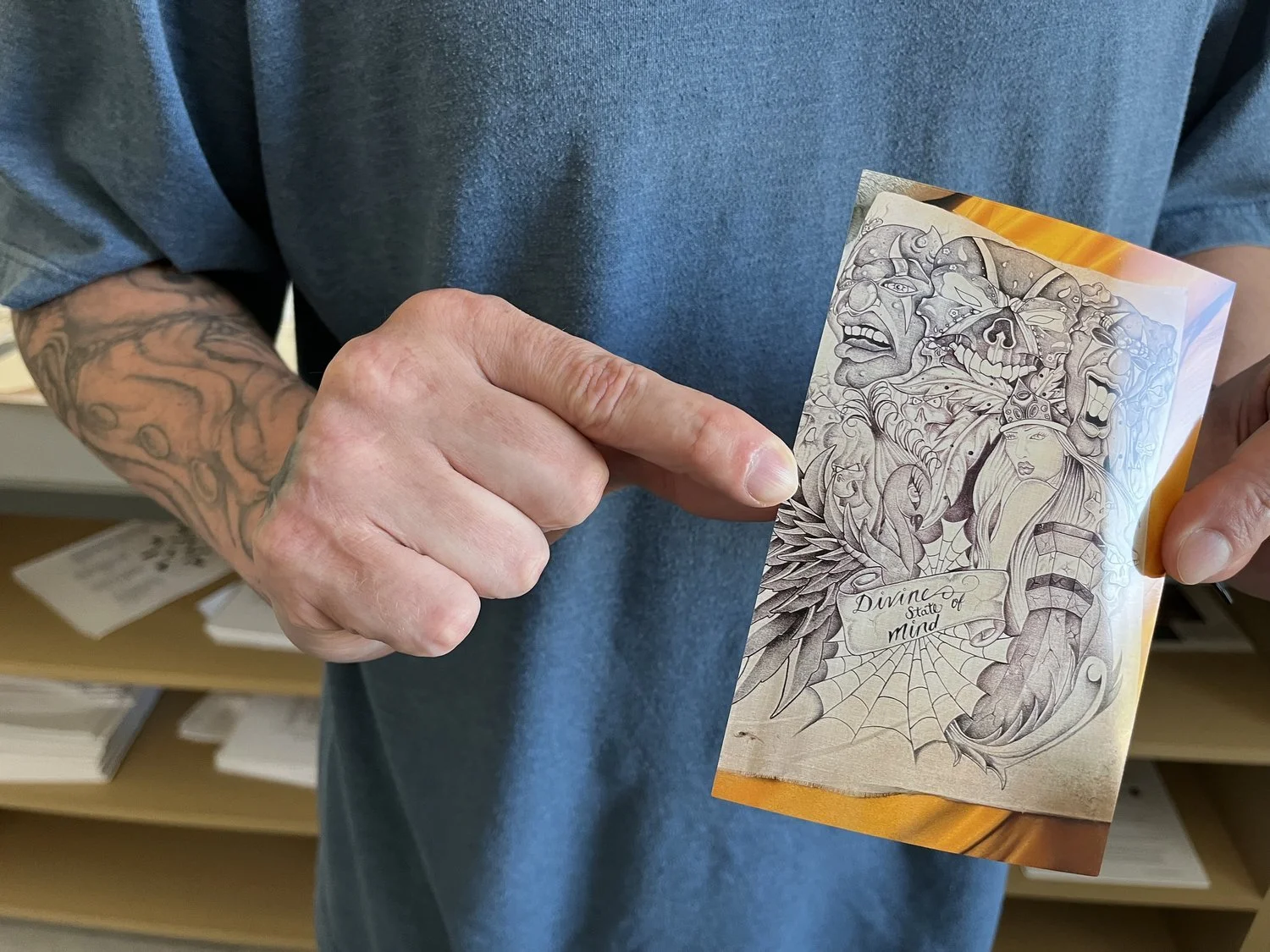
Douglas, a patient at Oregon State Hospital Salem, holds up the laminated copies of a “OSH Patient Rules Advisory Committee Notification” that were posted in the patient units regarding policy changes to patient personal property. According to Douglas, the phone number for the Zoom meeting did not work from the patient unit.
Following an inspection of OSH’s Junction City campus, the Centers for Medicare and Medicaid Services (CMS) produced a report outlining a number of concerns. In response, OSH began issuing a series of blanket policies across both campuses.
With patients at different stages of recovery at the hospital, some of these policies failed to consider the individual needs and progress of each patient’s treatment care plans. Treatment and clinical staff, who understand the potential impact a change can have on a treatment care plan, are not meaningfully included in the implementation of many policies. Patients are similarly not being meaningfully included.
Recommendations for Improvement
During Hospital Stay
The Oregon State Hospital should empower clinicians to provide patients the highest quality of care for the shortest time necessary. Patients at the hospital should expect therapeutic, evidence-based, and patient-centered treatment that is focused on recovery.
Follow Clinical Expert Recommendations & Individualized Treatment Care Plans
To ensure that individuals experience the highest quality of care and the shortest stays at the Oregon State Hospital, the executive team must not override the clinical discretion of the clinicians. While some patients may not be ready for certain privileges, other patients have worked hard to gain them. Removing privileges from patients who earned them over the course of their time at the hospital strips hope and their ability to effectively prepare for lives outside the hospital.
To restore continuity of the treatment care plans which have been disrupted by the Oregon State Hospital’s recent “environmental reset,” the Oregon State Hospital’s executive team should create and implement an accessible and timely system for patients to appeal these changes to their rights, privileges, and property allowances. The recommendations of the patient’s treatment team should guide these decisions.
Address Issues with Patient Medical Treatment
Patients are experiencing missed appointments and unclear communication regarding physical medical treatment. This is interfering with both their well-being and their mental health treatment.
OSH should review the current system for patients to receive physical healthcare. To better monitor and track delays and other obstacles related to the patients’ physical healthcare, the system should centralize all requests for evaluation, follow-up appointments, imaging, laboratory, and other specialist consultations.
Tailor Needs of the Most Acute Patients
To ensure that the most acute patients have individualized attention and clinically-based appropriate care, the hospital should work with staff to create a complex care unit. This unit would ensure that patients with the most significant needs can receive treatment appropriately tailored to their individual needs.
Implement Additional Intermediary Between Patients & Administrators
A member of the clinical staff on each unit should be appointed as the contact to be immediately notified if there is a conflict between orders from the executive team and the clinical judgment of the treatment team. Each of these instances should be tracked and reported. The hospital should mediate a solution to the conflict that prioritizes the well-being of the patient. Negative outcomes should be included in the tracking.
To ensure that patient perspectives are regularly reviewed by the executive team, we recommend more Patient Liaison roles within Oregon State Hospital. The Patient Liaison should spend time on units with patients to learn and understand the patient experience first-hand—then use this information to inform and advise the leadership team. This role should have separate oversight and authority from the existing OSH Ombuds Services & Friends and Family Services, which is currently identified as the patients’ liaison at Oregon State Hospital.
Re-Connect Patients with their Communities Outside
Patients correspond with friends, family, and supporters outside of the hospital via mail. Sometimes patients will purchase items from online retailers. Prior to the policy changes made in response to the CMS report, patients had the ability to send and receive packages. Patients earned this privilege.
Instead of developing thoughtful safety measures that would allow patients to receive packages from outside the hospital, OSH removed patient access to all packages, including from friends and family, except through specified retailers. Blanketly removing this privilege unnecessarily harms patients. OSH should employ whatever safety measures are necessary to allow patients to receive packages from outside of the hospital.
During the “Step Down” Process
Moving from a more to less restrictive level of placement—for example, from Oregon State Hospital to a secure residential location, then to an adult foster home or a residential treatment home—is a process called “stepping down.” Some people need more support than others during this process. Available case workers, or community navigators, could assist people in integrating back into the community before they leave the hospital.
Funding Supportive Housing & Case Management
To ensure patients’ stability and a successful transition back to Oregon communities, the Oregon Health Authority should immediately fund new community group-home or independent living placements for Guilty Except for Insanity (GEI) patients who are eligible to live in the community.
The hospital should then support every patient who has reached the end of jurisdiction under the Psychiatric Security Review Board with at least six months of housing and case management following their discharge from Oregon State Hospital. This is an important step in preventing homelessness.
Support Life in the Community, Not Life Behind Walls
When more of our behavioral health dollars are distributed to supporting home and community-based services, better options for recovery are made possible for everyone.
For example, funding a 24-hour per day dedicated staff member for a single resident in the community is substantially less expensive than housing a person at OSH. The approximate cost for an around the clock support staff dedicated to one person in an adult foster home is $12,000 per month. For comparison, the approximate cost of treatment for one person at Oregon State Hospital—which is the most restrictive environment—is $40,000 per month.
Investing in community-based services is a good use of Oregon’s General Fund. These investment are needed to prevent housing and community-based services from shutting down.
Review the Risk Review Process
The current Risk Review process is missing critical input from staff, patients, and community supporters. More transparency and consistency is needed in order to identify the obstacles that exist within the process.